This information serves as a guide to understanding the philosophy of harm reduction as it applies to offering Needle Syringe Program (NSP) services and is intended for existing or potential NSPs.
This guide supports the transfer of knowledge gained through research and experience to develop policies and procedures and deliver services. Evidence, best practices, and local context relevant to the North Bay Parry Sound district are reflected in this guide.
It is not intended to be a prescriptive set of practices for all NSP providers given the variations of scope and mandate across agencies.
Key Messages |
|
Background |
|
Concern regarding injection drug use, in the early 1990’s, led to the formation of a steering committee composed of members from the Addiction Research Foundation, AIDS Committee of North Bay & Area (ACNBA), North Bay and District Health Unit (NBDHU), and other community partners, known as CEDACON (Clean Exchange and Disposal Committee of North Bay). Funding was provided by the Public Health Branch to carry out a needs assessment. This led to the development of a delivery model, and in March 1999, North Bay’s first site opened at ACNBA. In early 2000, the Board of Health accepted the proposal for needle exchange program development, which became known as Northern Points Exchange (NPE). Four fixed sites in North Bay were established to provide Needle Exchange Services. Since then, the North Bay District and Parry Sound Health Units amalgamated, becoming the North Bay Parry Sound District Health Unit (NBPSDHU). Several more satellite Needle Syringe Program (NSP) sites have been established across the North Bay Parry Sound district. The term “exchange” is no longer used because the expectation of having used equipment to trade for new equipment can create barriers for people to access NSP services and can result in harm such as the reuse or sharing of used equipment. The NBPSDHU, which serves as the core NSP site for the district, receives harm reduction supplies from the Ontario Harm Reduction Distribution Program (OHRDP), purchases the remaining equipment (e.g., sharps containers, condoms, etc.), and distributes them to the satellite sites. The NBPSDHU is responsible for the submission of NSP distribution statistics for all sites in the district for ministry reporting, inventory management, and program planning and evaluation. Some information in this resource has been adapted from: |
Becoming a Satellite NSP Distribution Site |
|
Requests for new NSP sites are determined by consideration of various factors, which include but are not limited to:
Please contact us if you are interested in learning more. Join the Northern Points Community of Practice
|
The Philosophy of Harm Reduction |
|
Harm reduction programs and services are:
Harm reduction aims to reduce the negative health, social, and economic consequences associated with drug use. It includes a wide variety of practices, programs, and services that are evidence-based, client-centered, and meet people where they are “at”. Harm reduction makes no judgments or assumptions about the moral or legal nature of drug use and recognizes that substance use is complex. Harm Reduction ObjectivesThe main objectives of harm reduction practices are to reduce the individual, societal, and systemic risks associated with substance use, and optimize the health of clients. Reducing stigma associated with drug use is also an important part of harm reduction. Creating environments that foster respect and self-efficacy are conducive to individuals seeking further support and services available in the community based on personal readiness. Examples of Harm Reduction Approaches
Safer handling and disposal of used equipment is an important component of safer use education. |
Needle Syringe Programs |
Why do we need Needle Syringe Programs?Public Health is mandated by the Ministry of Health under the Ontario Public Health Standards (OPHS) to provide harm reduction services such as Needle Syringe Programs and naloxone. A central aim of the Infectious and Communicable Diseases Prevention and Control Program Standard, in relation to substance use, is to ensure access to sexual health and harm reduction services and supports that reduce or prevent exposure to and transmission of sexually transmitted infections (STIs) and blood borne Infections (BBIs). The provision of safer drug use equipment and safer use education reduces the spread of BBIs, such as Human Immunodeficiency Virus (HIV), Hepatitis B (HBV), and Hepatitis C (HCV) which otherwise can occur with sharing needles, straws, pipes, and other drug use equipment. Needle Syringe Programs, an important component of harm reduction approaches, are evidence-based and cost-effective in reducing the financial costs on the health care system related to treating BBIs and other health outcomes that require medical attention. The overall aim is to improve the health and well-being of individuals who use substances, increase access to services, and reduce the negative health, societal, and economic impacts of substance use. What are the Benefits of Offering Needle Syringe Programs?
|
Best Practice Recommendations |
Needle Syringe Programs (NSPs) operate based on the Best Practice Recommendations for Canadian Programs that Provide Harm Reduction Supplies to People Who Use Drugs and are at Risk for HIV, HCV, and Other Harms. Key information in this resource was drawn from this guidance document to ensure the appropriate operation and functioning of local NSPs.
What are Best Practices?Best practice recommendations apply to service design and delivery and are established by the best available evidence, and as such, are updated as new evidence emerges. The recommendations ensure that the needs of individuals who use drugs are met and that no inadvertent harm is done. Depending on the scope or mandate of the NSP-providing agency, some services or practices are not feasible, however consideration for the expansion of services should be made when and where possible. All agencies, regardless of the NSP services provided, offer a valuable connection to other health and social services in the community. What are the benefits of best practice recommendations?
Summary of Best Practice Recommendations
 |
Characteristics of Effective Programs |
Effective needle syringe programs are developed and implemented to meet the needs of the community. Characteristics of effective programs also include:
Achieving optimal, inclusive, and quality services
|
Safer Substance Use Equipment, Supplies and Distribution |
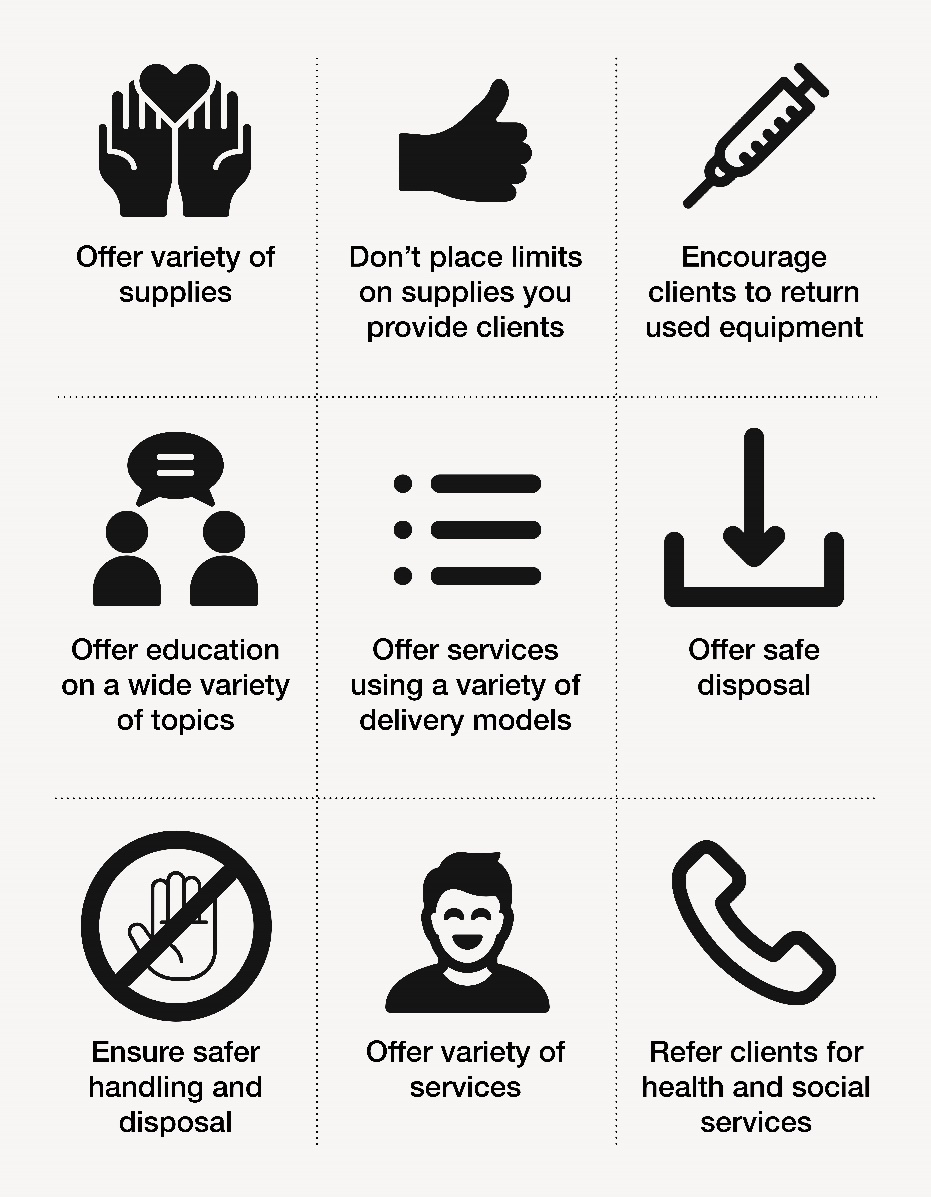
| Needle Syringe Programs (NSPs) should offer a wide variety of safer substance use supplies. The majority of the safer use equipment is funded through the Ontario Harm Reduction Distribution Program. Other items such as sharps containers, condoms, lubricant are purchased by the core site (Health Unit). Syringes/needles and biohazard sharps containers are purchased by the Health Unit for distribution to clients and satellite NSPs.
The items currently available to established satellite sites are found on the most recent NSP Supply Order Form. The order form is updated as the availability of supplies changes. Descriptions of the safer drug use equipment, and their purpose, are available in the Connecting Guide. Satellite sites are provided premade kits (e.g., injection, crystal meth, inhalation kits, etc.) or as bulk items. Standardized premade kits provide consistency and familiarity across the district although the contents may be changed by the core site based on local trends and client needs. It is recommended that NSPs provide supplies for safer sex practices, including:
Pre-made KitsSatellite sites in the North Bay Parry Sound District who order premade kits from the Health Unit, can expect to receive kits with the following counts and types of items depending on the kit type. The configuration of the kits is in the “background” of NEO, therefore when you track a premade kit, it counts all of the items contained in that kit. Bundles of the different coloured bags (empty) can be ordered in case your agency wishes to assemble some, although any changes to the contents should be discussed with your Health Unit contact person beforehand.
*Please note that the tubing for the mouthpieces for the straight stems and the bulb pipes are not the same size; be careful to keep them with their respective pipe type. Distribution of Safer Substance Use Equipment and SuppliesNSP supplies for people who use substances are offered in the quantities needed, wherever possible. Some of the supplies provided by NSPs are in high demand and we recognize that people, needing needles and sharps containers for medical injections, may struggle to find affordable or no-cost supplies. NSPs are funded only for supporting the needs of people who use substances. We respectfully direct people seeking medical supplies to their pharmacies, primary Health Care Providers, and specialty clinics for help with meeting their needs. Locations across Ontario that offer Needle Syringe Programs and community sharps bins can be found on the OHRDP’s Find Supplies map. Naloxone is distributed to individuals who use substances, or their family or friends across Ontario. Refer to this list of agencies that distribute naloxone in your community. |
Education and Other Services |
Safer Drug Use Education for ClientsSafer substance use education is an important part of harm reduction services. Providing new equipment and education on safer use practices go hand-in-hand. Safer use education should be offered in a variety of formats, wherever possible. This includes one-on-one education, workshops and group education, skill-building sessions, information pamphlets, instructional videos, demonstrations, targeted educational interventions (e.g., injection drug use, crack cocaine smoking) and other formats deemed necessary. Peer-delivered, brief interventions, and longer interventions should be offered to reach a broad range and diversity of clients. Safer Substance Use EducationSafer use of substances and equipment reduces the risk of bacterial infections and transmission of HIV, HBV, and HCV. Safer use education should include:
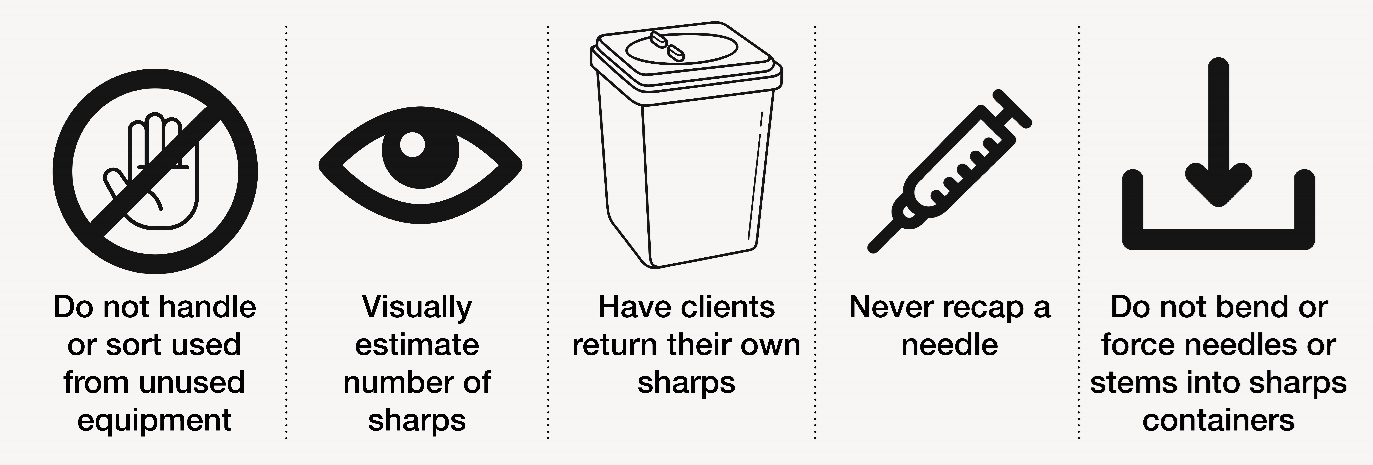
Handling and Disposal of Used EquipmentEducation on safer handling and disposal of used equipment includes placing sharps in a hard-sided container with a tight-fitting lid such as a bleach bottle, coffee tin, or plastic pop bottle when a biohazardous waste container is not available. All other waste should be disposed of in garbage receptacles out of reach of children and pets. There is more information on sharps handling and disposal on our health unit website. Staff at NSPs should consider the following when receiving used sharps and drug use equipment for disposal:
Accidental Sharps InjuryNSPs should have their own occupational health and safety response plans related to accidental sharps injuries. Some information is available about sharps injuries, however advice from a medical professional should be sought for assessment and recommendations related to post-exposure prophylaxis (PEP). Education and Training for Staff at Needle Syringe ProgramsNSP staff are foundational to offering warm, welcoming, and non-judgmental settings for clients. Understanding and consistently representing the principles of harm reduction are important to working with people who use substances and other marginalized populations. Reliable sources for learning and for professional development include:
Other Harm Reduction Programs and ServicesOpioid Overdose/Toxicity ResponseNaloxone is distributed at some NSP sites. Please see the Ontario Naloxone Program (ONP) website for information on eligibility criteria. Our health unit website also has general information on naloxone as well as information for ONP Distributing Agencies and First Responders. |
Used in the Development of this Resource |
|
Additional Resources |
|
Questions, concerns or feedback about harm reduction services?